The
protected health information of nearly 80,000 patients of Fertility
Centers of Illinois (FCI) may have been pawed over by cyber intruders
following a cyberattack.
FCI runs four clinics across Illinois. According to
the U.S. Department of Health and Human Services (HHS) Office for Civil
Rights’ data breach site, the breach – reported on Dec. 27 – affected
79,943 people.
FCI’s data breach notice (PDF)
said that the healthcare organization first detected suspicious
activity on its internal systems on Feb. 1, 2021. A subsequent
investigation indicated that security systems had blocked attackers from
accessing patient EMR (electronic medical records) systems. However,
the intruder(s) managed to access administrative files and folders.
FCI said that it immediately launched a “thorough and comprehensive
review” of its records to identify the files accessed, the information
contained in those files and the individuals to whom that information
pertained.
By Aug. 27, 2021, FCI had determined that information related to
certain FCI patients was included in the set of files that had been
improperly accessed. One positive finding so far: FCI said it’s “not
aware of any actual or attempted misuse of patient information as a
result of this incident.”
May it stay that way, given the severe harm that could be done with
the dizzying array of highly sensitive personally identifying
information (PII) that was involved: a trove that could be mined for
financial fraud, identity theft, healthcare fraud and more.
A Treasure Trove of Compromised Data
The accessed files included some patients’ names, employer-assigned
ID numbers, passport numbers, Social Security numbers, financial account
information, payment card information, treatment information,
diagnosis, treating/referring physicians, medical record number, medical
billing/claims information, prescription/medication information,
Medicare/Medicaid identification information, health insurance group
numbers, health insurance subscriber numbers, patient account numbers,
encounter numbers, ill health/retirement information, master patient
index, occupational-health related information, other medical benefits
and entitlements information, other medical ID numbers, patkeys/reason
for absence, sickness certificate, usernames and passwords with PINs or
account login information, and medical facilities associated with
patient information.
The Big Business of Extremely Intimate Data
Stealing this kind of data is big business. One example: In October, a Las Vegas man and former medical records tech was sentenced
to 12.5 years of prison for stealing PII that was then used to
fraudulently claim Department of Defense (DoD) and Veterans
Administration (VA) benefits, particularly targeting disabled veterans.
The data of more than 3,300 U.S. military service members, military
dependents and civilians employed by the DoD were compromised as part of
what turned out to be a transnational cybercrime ring created to
defraud them out of $1.5 million in military benefits from the DoD and
the VA.
With regards to the FCI breach, the organization said that it
immediately took steps to eliminate unauthorized access and brought in
independent forensic investigators to investigate and remediate the
matter, on top of additional security measures meant to further secure
access to data, individual accounts, and equipment, including the
implementation of enterprise identity verification software.
FCI has also bolstered employee security practices training and has
offered a year’s worth of free credit monitoring and identity theft
protection through Equifax.
“Please be assured that we have invested considerable resources to
ensure that such a vulnerability does not exist in the future,” FCI
concluded.
The New Year Has Had a Lot of Picking On Patients
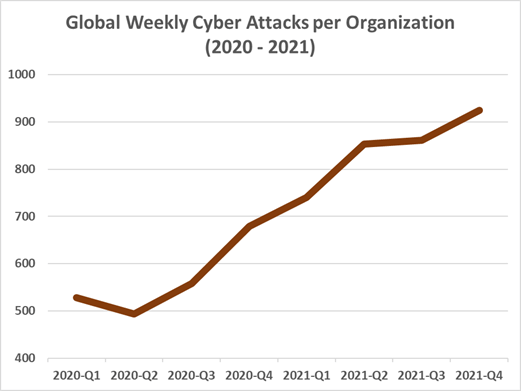
Easier said than done, apparently. Unfortunately, the new year has ushered in an undiminished zest for attacking healthcare information.
Earlier this week, Florida’s Broward Health System announced that the most intimate medical data of 1,357,879 patients was breached
in October: evidence of what security researchers said is a
soft-bellied healthcare software supply chain that’s proved to be a
juicy target for cybercriminals.
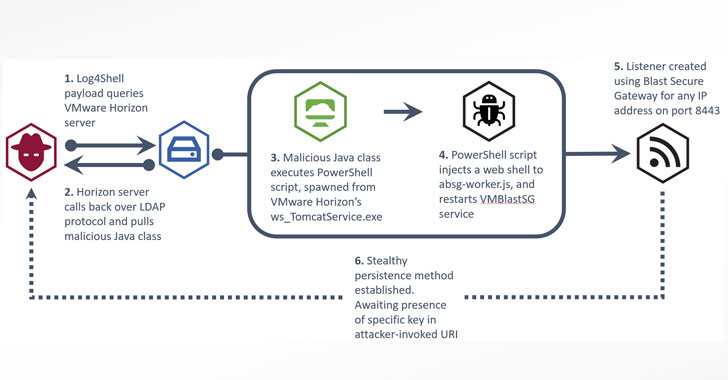
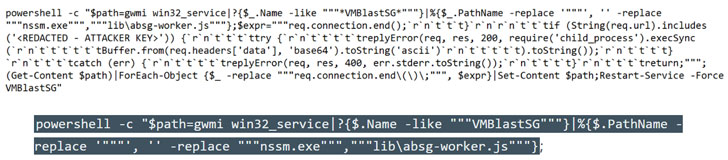
Healthcare organizations are also in the same log-jammed boat as
every other sector: They’re hyper-focused on mitigating threats
associated with the Apache Log4j vulnerability and trying to avoid the disastrous consequences if the Log4Shell flaws are exploited.
Earlier this week, Microsoft reported that it saw rampant Log4j exploit attempts and testing through the end of December.
The Acute Danger of Log4j for Healthcare
On Dec. 17, a week after the discovery of the Log4j flaw, the HHS 405(d) Task Group issued a brief (PDF)
outlining the risks associated with the vulnerability that could have
catastrophic security implications for healthcare and other sectors.
“The exploitation allows the execution of any code which could result
in compromise of the server, download of malicious binaries, or
propagation of further attacks such as ransomware or a zero-day attack,”
according to HHS’s alert.
It’s not even clear how many healthcare systems and devices could be
affected by Log4Shell or what all the ways of exploitation might be, but
it’s estimated that it could potentially affect hundreds of millions of
devices, networks and/or software platforms, HHS said.
“Healthcare organizations are dependent on readily available devices
and software that are vendor-supplied and connected to an external
network to operate. These complex and interconnected devices affect
patient safety and privacy,” according to HHS.
“They represent potential attack vectors across an organization like
medical equipment such as bedside monitors that monitor vital signs
during an inpatient stay,” the alert continued. “Or, they may be more
complicated, like infusion pumps that deliver specialized therapies and
require continual drug library updates. If an attacker gained access to
the network through a vulnerability such as Log4j, they would be able to
gain control of the software and could potentially disconnect devices
from the network, therefore, causing a disruption to daily procedures
and putting patient safety at risk.”
HHS explained that mainstream and well-known organizations, including
cloud services, use Log4j software and may be vulnerable, including
cloud applications that medical organizations use for Electronic Health
Records (EHR) services and outsourced security services such as Software
as a Service (SaaS).
Github maintains a running list of affected services and products.
Admin Account Used to Get at Data
Ben Pick, Principal Consultant at app security provider nVisium,
noted that FCI stated that it followed reasonable practices to protect
users and that an administrative account was used to obtain the data:
the privileged kind of account from which attackers can do beaucoup
damage. “These higher privileged accounts often have access to
widespread data and act as a single point of failure, as evidenced by
the large amount of user data exposed,” he told Threatpost via email.
His advice, in lieu of knowing the cause of the administrator’s
account being compromised, is to limit access rights based on need to
know.
Failing that, monitor, monitor, monitor, Pick advised: “When these
privileged accounts cannot be limited, then strong monitoring must be
enforced. This would alert when anomalous calls are made to indicate
when an administrator may be performing an excessive amount of searches
and possibly exfiltrating data.”
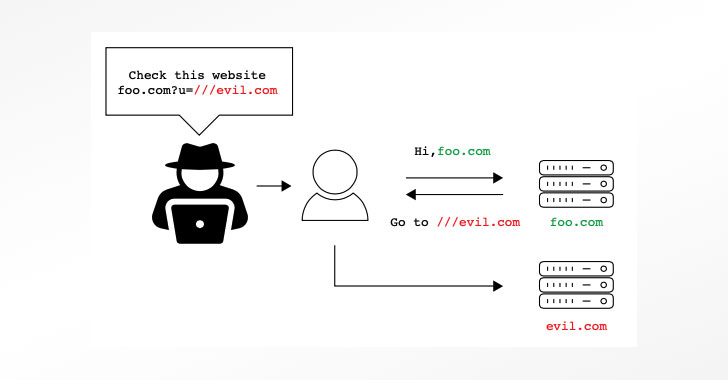
The Soft Spot of APIs
Mac McMillan, CEO of CynergisTek, predicted in an interview
with HealthITSecurity that in the new year, ransomware operators will
shift their focus away from encryption and on to data exfiltration.
Blame the soft spot of APIs, he said: “As interoperability becomes
more of a mainstream priority for healthcare organizations and we see
more APIs that are being introduced between critical systems, I think
we’re going to see a rise in the number of attacks that are focused on
compromising those APIs.
“It’s another area where [we] don’t typically have a good, consistent
approach across the board in healthcare with respect to testing APIs
for security.”
This is particularly true given that healthcare organizations are now
looking at an API change-over deadline: By year’s end – Dec. 31, 2022 –
they’re required to migrate to Fast Healthcare Interoperability Resources
(FHIR) APIs in order to enable seamless data sharing. Implementing the
new data standards will likely cause enough turmoil that threat actors
will be that much more attracted to APIs as a network entry point, McMillan suggested.
Why Was FCI’s Regulated Data Outside of Network Monitoring?
Jake Williams, Co-Founder and CTO at incident response firm BreachQuest,
noted to Threatpost on Friday that it’s not uncommon for medical
organizations to store patient data outside of their EHR system, and it
sounds like that’s what happened here.
“As the article notes, the EMR was not compromised due to unspecified security measures,” Williams said via email.
“However, files (presumably on some network share) were accessed by
threat actors. It wouldn’t surprise me to learn that the EMR enforces
[multi-factor authentication] or doesn’t use domain authentication.”
Williams suggested that organizations take inventory of where they
may have regulated data that may fall outside of normal monitoring and
audit controls: a topic that Citrix iterated in a September sponsored article on Threatpost.
“Those who don’t perform regular data inventory searches almost
certainly have regulated data in their file shares – a location where it
is just one phishing email away from compromise,” Williams said.
_Photo courtesy of _Marko Milivojevic via Pixnio. Licensing details.